Conditions
Pterygium (Surfer’s Eye)
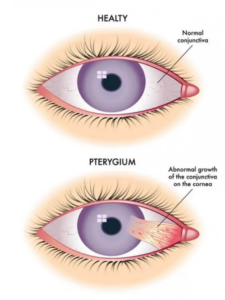
Pterygium is a growth of fleshy tissue on the conjunctiva (the clear membrane covering the white part of the eye) that can extend onto the cornea.
Book an appointment.
Consult our expert team to discover if cataract surgery can restore your crystal-clear vision and learn about the advanced lens options that can enhance your sight.
appointments
Would you like to speak with someone to schedule your appointment?
+960 332 1026
Feedbacks
Do you have some feedback for us in mind? Please send us an email message.
Suitability self test.
Take our quick Suitability Self-Test to see if you're a potential candidate for surgery.
Pterygium Incidence/Prevalence
Pterygium is a growth of fleshy tissue on the conjunctiva (the clear membrane covering the white part of the eye) that can extend onto the cornea. It is commonly referred to as “surfer’s eye” because it often occurs in people who spend a lot of time outdoors, particularly in sunny, windy, or dusty environments. Studies show higher prevalence rates among people aged 40 and older, often exceeding 10% in older adults. It is more commonly seen in males than females, likely due to higher exposure to outdoor environments.

Pterygium Causes
- Ultraviolet (UV) Light Exposure
- Sunlight: Prolonged exposure to UV rays from the sun is the most significant risk factor for pterygium. People who spend a lot of time outdoors, especially in sunny climates, are at higher risk.
- Environmental Irritants
- Dust and Wind: Exposure to wind, dust, sand, and other environmental irritants can contribute to the development of pterygium, particularly in occupations or activities that involve outdoor work.
- Genetic Factors
- Family History: A genetic predisposition may increase susceptibility to pterygium, suggesting a hereditary component.
- Age
- Older Adults: The risk of developing pterygium increases with age, as cumulative UV exposure over time contributes to its formation.
- Gender
- Males: Men are more likely to develop pterygium than women, likely due to higher outdoor activity levels.
- Previous Eye Conditions
- Irritation or Injury: Previous eye conditions or injuries that cause irritation may predispose individuals to developing pterygium.
Pterygium Diagnosis and Examination Process
- Patient History
- Symptoms: The doctor will ask about any symptoms, such as redness, irritation, or visual disturbances.
- Risk Factors: Discussion of environmental exposure (e.g., UV light, wind, dust) and any family history of eye conditions.
- Visual Acuity Test
- This initial test assesses how well you can see at various distances, usually using an eye chart.
- Slit-Lamp Examination
- A slit lamp is a microscope with a bright light that allows the doctor to examine the front structures of the eye, including the conjunctiva and cornea. This is the primary tool for diagnosing pterygium.
- The doctor will look for:
- The presence of a fleshy growth on the conjunctiva.
- The extent to which the growth has invaded the cornea.
- Assessment of Symptoms
- The doctor may assess the degree of irritation or inflammation associated with the pterygium.
- Photodocumentation
- In some cases, photographs may be taken for further evaluation or to track changes over time.
- Additional Tests (if necessary)
- While not typically required for pterygium, other tests may be conducted to rule out other conditions if there are atypical findings or symptoms.
Pterygium Treatments
Treatment for pterygium depends on the severity of the growth and the symptoms experienced by the patient. Here are the main treatment options:
- Observation
- Indication: If the pterygium is small and asymptomatic, regular monitoring may be sufficient. No immediate treatment is needed unless it progresses.
- Medications
- Artificial Tears: Over-the-counter lubricating eye drops can help relieve dryness and irritation caused by pterygium.
- Anti-Inflammatory Drops: Prescription eye drops may be used to reduce inflammation and redness.
- Surgical Removal
If the pterygium causes significant discomfort, affects vision, or continues to grow, surgery may be recommended. Surgical options include:
- Excision: The pterygium is surgically removed from the conjunctiva and cornea.
- Conjunctival Grafting: This technique involves taking a small piece of conjunctiva (the membrane covering the eye) from another part of the eye and placing it over the area where the pterygium was removed. This method reduces the risk of recurrence.
- Post-Surgery Care
- Follow-Up: Regular follow-up appointments are important to monitor healing and check for any recurrence.
- Protective Eyewear: Patients may be advised to wear sunglasses with UV protection to prevent reformation, especially in sunny environments.
- Recurrence Prevention
- In some cases, additional treatments like topical mitomycin C or anti-inflammatory medications may be used post-surgery to help prevent recurrence.
Pterygium FAQs
What are the symptoms of pterygium?
Common symptoms include:
- Redness and irritation in the eye.
- A visible fleshy growth on the white part of the eye.
- A sensation of something in the eye.
- Blurred vision if it extends over the cornea.
Is pterygium serious?
- While pterygium is generally not serious, it can lead to discomfort, irritation, and vision problems if left untreated. In rare cases, it may recur after surgery.
Does pterygium require surgery every time?
Not necessarily. Many cases of pterygium can be managed with observation and medication, especially if they are small and asymptomatic. Surgery is usually reserved for more severe cases.
What is the recovery process like after pterygium surgery?
Recovery typically involves:
- Taking prescribed eye drops to manage inflammation and discomfort.
- Avoiding strenuous activities and eye strain.
- Regular follow-up visits to monitor healing.
Can lifestyle changes help manage pterygium?
Yes, lifestyle changes can help manage and reduce symptoms. These include:
- Wearing sunglasses with UV protection.
- Staying hydrated.
- Avoiding environments with high dust or wind exposure.
Can pterygium affect both eyes?
Yes, pterygium can occur in one or both eyes. It’s not uncommon for individuals to develop pterygia in both eyes, particularly if they share common risk factors.

